Abstract
Dietary calcium intake and mortality risk from cardiovascular disease and all causes: a meta-analysis of prospective cohort studies.
Considerable controversy exists regarding the association between dietary calcium intake and risk of mortality from cardiovascular disease and all causes. Therefore, we performed a meta-analysis of prospective cohort studies to examine the controversy.
We identified relevant studies by searching MEDLINE, Embase, and the Cochrane Library databases between 1 September 2013 and 30 December 2013. Reference lists of relevant articles were also reviewed. Observational prospective studies that reported relative risks and 95% confidence intervals for the association of calcium intake with cardiovascular and all-cause mortality were eligible. Study-specific relative risks were pooled using a random-effects model.
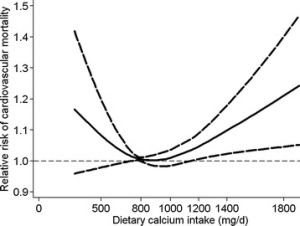
In this meta-analysis, 11 prospective studies with 12 independent cohorts, involving 757,304 participants, were eligible. There was evidence of a non-linear association between dietary calcium intake and risk of mortality from cardiovascular disease (P for non-linearity <0.01) and all causes (P for non-linearity <0.01). A dose-response analysis showed a U-shaped relationship between dietary calcium intake and cardiovascular mortality. Intakes that were lower and higher than around 800 mg/day were gradually associated with a higher risk of cardiovascular mortality. For all-cause mortality, we also observed a threshold effect at intakes around 900 mg/day. The risk of all-cause mortality did not decrease further at intakes above 900 mg/day.
This meta-analysis of prospective cohort studies suggests that dietary calcium intake is associated with cardiovascular mortality in a U-shaped manner and that high dietary calcium intake (>900 mg/day) is not associated with a decreased risk of all-cause mortality.
Wang X, Chen H, Ouyang Y, Liu J…
BMC Med 2014
PMID: 25252963 | Free Full Text
From the full text: